Discussion
The correct answer is D. This is a translocation RCC.
This case represents a TFE3-rearranged renal cell carcinoma (RCC), also referred to as Xp11 translocation RCC, since the translocation occurs on the X-chromosome, specifically at Xp11. The morphology in this case shows the characteristic histologic features of a translocation RCC; the tumor exhibits papillary and solid alveolar growth with high-grade epithelioid clear cells and numerous scattered psammoma bodies. Fluorescent in-situ Hybridization (FISH) testing performed on formalin-fixed paraffin-embedded tissue sections confirmed the TFE3 rearrangement.
Xp11 translocation RCC is one of several renal cell tumors defined by its molecular characteristics, according to the 2021 World Health Organization (WHO) Classification of Renal Tumors. Other such molecularly-defined renal tumors include: TFEB-altered RCC, where the translocation is at 6p21; ELOC (formerly TCEB1)-mutated RCC, with the mutation at 8q21; Fumarate hydratase (FH)-deficient RCC, mutated at 1q43; Succinate dehydrogenase (SDH)-deficient RCC, where the mutation could be any four of the SDH-complex genes, SDHA, SDHB, SDHC, and SDHD (most commonly SDHB at 1p36); ALK-rearranged RCC, with gene fusions at 2p23; and SMARCB1-deficient renal medullary carcinoma, with deletion or translocation at 22q11. The Xp11 translocation RCCs have gene fusions involving TFE3 which (along with TFEB) is part of the microphthalmia-associated (MiT) family of transcription factors. As such, the tumor in this case is sometimes referred to as part of the MiT family translocation RCCs.
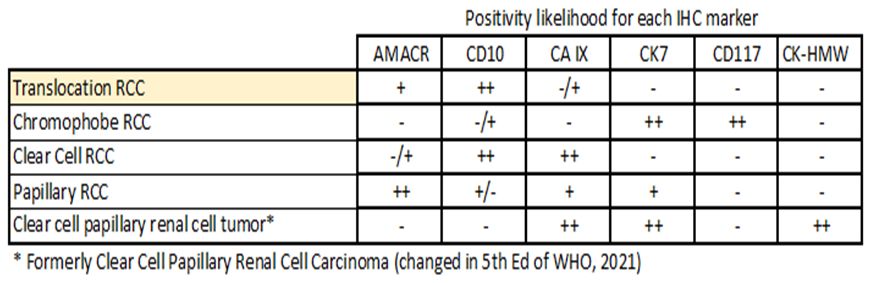
TFE3-rearranged RCCs often have papillary, alveolar, and nested growth patterns with clear and eosinophilic cells. The neoplastic cells show high grade nuclei. Psammoma bodies are frequently present, and melanin pigment may be seen. The tumors are more common in children and young adults, and more often found in females. They encompass approximately 40% of pediatric RCCs and 3% of RCCs in adults. One risk factor is exposure to cytotoxic chemotherapy. The expected Immunohistochemical (IHC) profile for this tumor, and other renal tumors in the differential diagnosis, is as follows:
Discussion on the differential diagnosis:
Chromophobe RCC – Histologically, there is proliferation of compact cells with finely reticulated pale cytoplasm and prominent cell membranes. “Koilocytic” nuclear atypia with wrinkled nuclear membranes (raisinoid appearance) and perinuclear halos is typical, and binucleation is common. IHC staining shows diffuse CD117 and CK7 staining; CD10 is typically negative.
Clear cell RCC – On histologic examination, no true papillae are seen, but rather alveolar nests and sheets of clear cells interspersed by a delicate vascular network are present. IHC staining shows diffuse CA IX positivity, with AMACR more likely to be negative.
Papillary RCC – The histologic features show papillae and tubulopapillary structures with true fibrovascular cores. If a solid pattern is seen, it is due to tightly compact growth of papillae. Foamy histiocytes expanding papillary cores are characteristic. There are no nested alveolar patterns and no extensive areas of clear cells as seen in translocation RCC. There are two subtypes: Type-I shows papillae lined by a single layer of cells, usually with low-grade nuclear features and scant cytoplasm; Type-II shows pseudostratified nuclei of higher grade and abundant eosinophilic cytoplasm. IHC staining reveals CK7 positivity in 80% of type I, but only 20% of type II tumors.
Clear cell papillary renal cell tumor – The tumor is mainly composed of cells with clear cytoplasm arranged in papillary, tubular, and solid patterns. The nuclei are low grade. No psammoma bodies/ calcifications are present. IHC stains reveal CK7, CA IX, and CK-HMW positivity; CA IX shows a “cup-like” staining pattern. AMACR and CD10 are typically negative.
References:
WHO, 5th Edition: https://tumourclassification.iarc.who.int/chaptercontent/36/25
Klatte T, et al. Renal cell carcinoma associated with transcription factor E3 expression and Xp11.2 translocation: incidence, characteristics, and prognosis. Am J Clin Pathol. 2012 May;137(5):761-8. doi: 10.1309/AJCPQ6LLFMC4OXGC. PMID: 22523215
Komai Y, et al. Adult Xp11 translocation renal cell carcinoma diagnosed by cytogenetics and immunohistochemistry. Clin Cancer Res. 2009 Feb 15;15(4):1170-6. doi: 10.1158/1078-0432.CCR-08-1183. PMID: 19228722.
Rao Q, et al. Renal cell carcinoma in children and young adults: clinicopathological, immunohistochemical, and VHL gene analysis of 46 cases with follow-up. Int J Surg Pathol. 2011 Apr;19(2):170-9. doi: 10.1177/1066896909354337. Epub 2009 Dec 24. PMID: 20034980.
Argani P. MiT family translocation renal cell carcinoma. Semin Diagn Pathol. 2015 Mar;32(2):103-13. doi: 10.1053/j.semdp.2015.02.003. Epub 2015 Feb 4. PMID: 25758327.
Argani P, et al. Xp11 translocation renal cell carcinoma in adults: expanded clinical, pathologic, and genetic spectrum. Am J Surg Pathol. 2007 Aug;31(8):1149-60. doi: 10.1097/PAS.0b013e318031ffff. PMID: 17667536.
Meyer PN, et al. Xp11.2 translocation renal cell carcinoma with very aggressive course in five adults. Am J Clin Pathol. 2007 Jul;128(1):70-9. doi: 10.1309/LR5G1VMXPY3G0CUK. PMID: 17580272.
Argani P, et al. Renal carcinomas with the t(6;11)(p21;q12): clinicopathologic features and demonstration of the specific alpha-TFEB gene fusion by immunohistochemistry, RT-PCR, and DNA PCR. Am J Surg Pathol. 2005 Feb;29(2):230-40. doi: 10.1097/01.pas.0000146007.54092.37. PMID: 15644781.
Reddy, V et al. Gattuso’s Differential Diagnosis in Surgical Pathology. 4th ed. Elsevier Health Sciences; 2021. pp. 518-519, 521, 529. Available online at: https://bookshelf.health.elsevier.com/reader/books/9780323661676/epubcfi/6/94[%3Bvnd.vst.idref%3DB9780323661652000107]!/4/2/4[B9780323661652000107]/1:25[ina%2Cry%20]
Immunoquery: https://app.immunoquery.com/main
Board Review Type Questions
1. Which of the following is true regarding MiT-family translocation renal cell carcinomas?
A. More common in older adults
B. More common in males
C. TFEB-rearrangement is more common than TFE3-rearrangement
D. TFEB-rearrangement RCC shows characteristic raisinoid nuclei and prominent cell
membranes
E. The TFE3-rearrangement occurs at the Xp11 breakpoint
2. Which of the following is the correct chromosome abnormality for the molecularly-defined RCC?
A. TFEB-altered RCC - Xp11
B. TFE3-rearranged RCC – 6p21
C. ALK-rearranged RCC – 2p23
D. ELOC (formerly TCEB1)-mutated RCC – 22q11
E. SMARCB1-deficient renal medullary carcinoma – 8q21
The correct answer is E. The TFE3-rearrangement occurs at the Xp11 breakpoint.
A and B are incorrect because the MiT family RCCs are more common in children/young adults & females.
C. The opposite is true. TFE3 is more common in MiT-family translocation RCC. The correct answer is E. he TFE3-rearrangement occurs at the Xp11 breakpoint.
D. These are histologic features on chromophobe RCC not MiT-family translocation RCC.
The correct answer is C. ALK-rearranged RCC – 2p23
The answers for A and B are switched . TFEB-altered RCC has the alteration at 6p21; TFE3-rearranged RCC occurs at Xp11.
Answers D and E are also switched. ELOC-mutated RCC has the mutation occurring at 8q21; SMARCB1-deficienty renal medullary carcinoma has a deletion or translocation at 22q11
